Source: Nature News
Before committing suicide at the age of 22, an anonymous man with schizophrenia donated a biopsy of his skin cells to research. Reborn as neurons, these cells may help neuroscientists to unpick the disease he struggled with from early childhood.
Experiments on these cells, as well as those of several other patients, are reported today in Nature1. They represent the first of what are sure to be many mental illnesses 'in a dish', made by reprogramming patients' skin cells to an embryonic-like state from which they can form any tissue type.
Recreating neuropsychiatric conditions such as schizophrenia and bipolar disorder using such cells represents a daunting challenge: scientists do not know the underlying biological basis of mental illnesses; symptoms vary between patients; and although psychiatric illnesses are strongly influenced by genes, it has proved devilishly hard to identify many that explain more than a fraction of a person's risk.
"All of us had been contacted by patients asking 'when can I get my stem cells to solve my schizophrenia'. It's not as simple as that," says Russell Margolis, a psychiatrist and neurogeneticist at Johns Hopkins University in Baltimore, Maryland, who was not involved in the study. "It's an additional piece to the puzzle as opposed to the answer."
Cocktail recipe:Before committing suicide at the age of 22, an anonymous man with schizophrenia donated a biopsy of his skin cells to research. Reborn as neurons, these cells may help neuroscientists to unpick the disease he struggled with from early childhood.
Experiments on these cells, as well as those of several other patients, are reported today in Nature1. They represent the first of what are sure to be many mental illnesses 'in a dish', made by reprogramming patients' skin cells to an embryonic-like state from which they can form any tissue type.
Recreating neuropsychiatric conditions such as schizophrenia and bipolar disorder using such cells represents a daunting challenge: scientists do not know the underlying biological basis of mental illnesses; symptoms vary between patients; and although psychiatric illnesses are strongly influenced by genes, it has proved devilishly hard to identify many that explain more than a fraction of a person's risk.
"All of us had been contacted by patients asking 'when can I get my stem cells to solve my schizophrenia'. It's not as simple as that," says Russell Margolis, a psychiatrist and neurogeneticist at Johns Hopkins University in Baltimore, Maryland, who was not involved in the study. "It's an additional piece to the puzzle as opposed to the answer."
Since researchers reported that cocktails of particular genes can be used to reprogram human cells to an embryonic-like state2,3, scientists have learned to coax these 'induced pluripotent stem cells' (iPSCs) into various cell types and used them to try to work out what goes awry in disease. So far, iPSC-derived models have been published for about a dozen diseases, from rare heart conditions4,5 to hereditary blood diseases6.
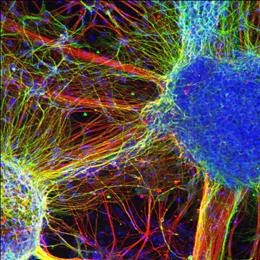
Fred Gage, a neuroscientist at the Salk Institute for Biological Studies in San Diego, California, and his team created iPSC models from the cells of the 22-year-old man mentioned above, as well as those of two brother–sister pairs, all of whom had either schizophrenia or related conditions such as schizoaffective disorder.
When the authors transformed the iPSCs into neurons, they noticed that the patient-derived cells made fewer connections, or synapses, with other neurons in the same dish than did neurons from people without psychiatric disorders. However, tests showed that the patients' neurons conducted electrical pulses just as well as normal neurons did.
Interestingly, the antipsychotic medication loxapine, used to treat schizophrenia, boosted the number of synapses formed by the patient-derived neurons to normal levels.
Four other antipsychotic drugs had no consistent effect, although Gage notes that all of the drugs benefited cells from at least one patient. His team also reported differences in gene expression between the neurons of patients with schizophrenia and those of healthy people, including changes in genes related to synapse function and others previously implicated in genetic studies of the disease.

No comments:
Post a Comment